 |
| (c) Cornell Univ |
Please read the disclaimer here.
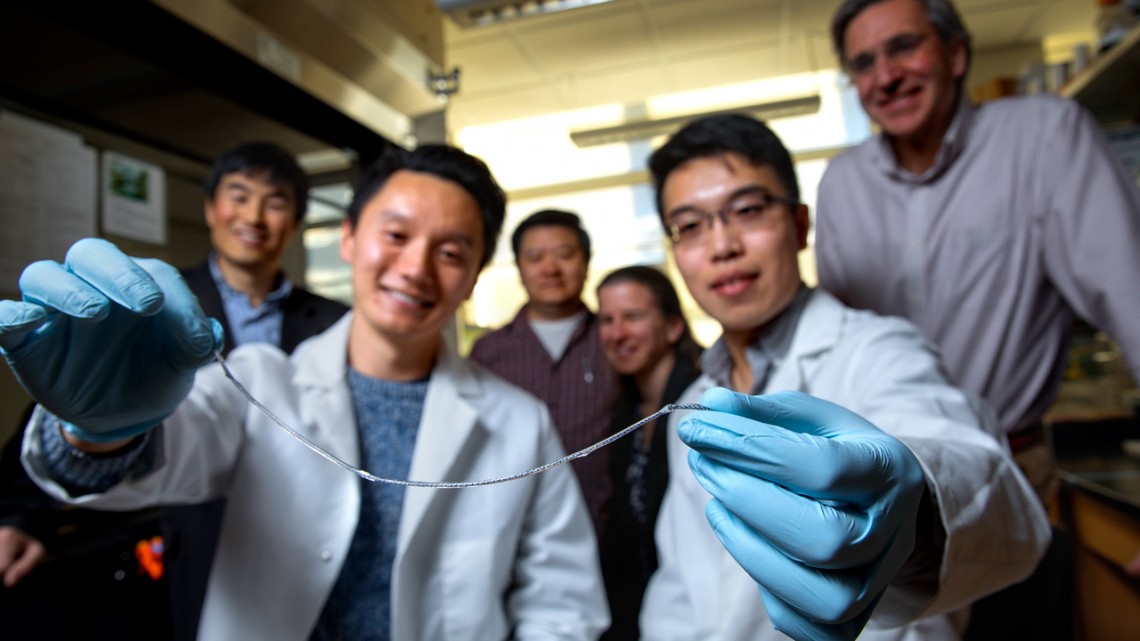
In Type 1 diabetes, insulin-producing pancreatic cell clusters (islets) are destroyed by the body’s immune system. The research group, led by assistant professor Minglin Ma from the Department of Biological and Environmental Engineering in the College of Agriculture and Life Sciences at Cornell, has devised an ingenious method for implanting hundreds of thousands of islet cells into a patient. They are protected by a thin hydrogel coating and, more importantly, the coated cells are attached to a polymer thread and can be removed or replaced easily when they have outlived their usefulness.
Transplantation of stem cell-derived, insulin-producing islet cells is an alternative to insulin therapy, but that requires long-term immunosuppressive drug administration. One well-researched approach to avoid the immune system’s response is to coat and protect the cells in tiny hydrogel capsules, hundreds of microns in diameter. However, these capsules cannot be taken out of the body easily, since they’re not connected to each other, and there are hundreds of thousands of them. And the ability to remove the transplant is key because of the potential of tumors forming when stem cell-derived, insulin-producing cells – the most promising cell source for type 1 diabetes cell therapies – are used.
 |
| (c) Wikipedia |
That string: an ionized calcium-releasing, nanoporous polymer thread. The device starts with two sterile nylon sutures twisted in a helix, then folded over to facilitate the subsequent nanoporous structure coatings. Placed onto that thread is a thin layer of islet cell-containing alginate hydrogel, which adheres to the helical, nanoporous thread, similar to dew drops sticking to the spider silk. Alginate is a seaweed extract commonly used in encapsulated cell transplantation.
This thread – which the group has dubbed TRAFFIC (Thread-Reinforced Alginate Fiber For Islets enCapsulation) – was inspired by a spider’s web but is even better because the hydrogel covers the thread uniformly. And since the thread is twisted and porous, the hydrogel won’t slip off as it would on a single, smooth piece of material.
This therapy would involve minimally invasive laparoscopic surgery to implant approximately six feet of hydrogel-coated thread into the patient’s peritoneal cavity.
TRAFFIC’s large surface area promotes better mass transfer, and diffusion is good because all the islet cells are near the surface. Current life span estimates for the thread are between six and 24 months, although more testing is necessary.
In mice, blood glucose levels were returned to normal two days after implantation of a one-inch length of TRAFFIC, and remained normal for at least three months when the experiment ended. Retrievability was tested in multiple dogs, with 10-inch samples being successfully implanted and removed laparoscopically.
This work was supported by the American Diabetes Association, the Cornell Technology Acceleration and Maturation Fund, and the Cornell Stem Cell Program Seed Fund. The work made use of the Cornell Center for Materials Research shared facilities, which are supported by the National Science Foundation.
Source, PNAS
No comments:
Post a Comment